 Bronchiectasis is a chronic and progressive inflammatory disease often marked by unpredictable exacerbations 1
Bronchiectasis is a chronic and progressive inflammatory disease often marked by unpredictable exacerbations 1
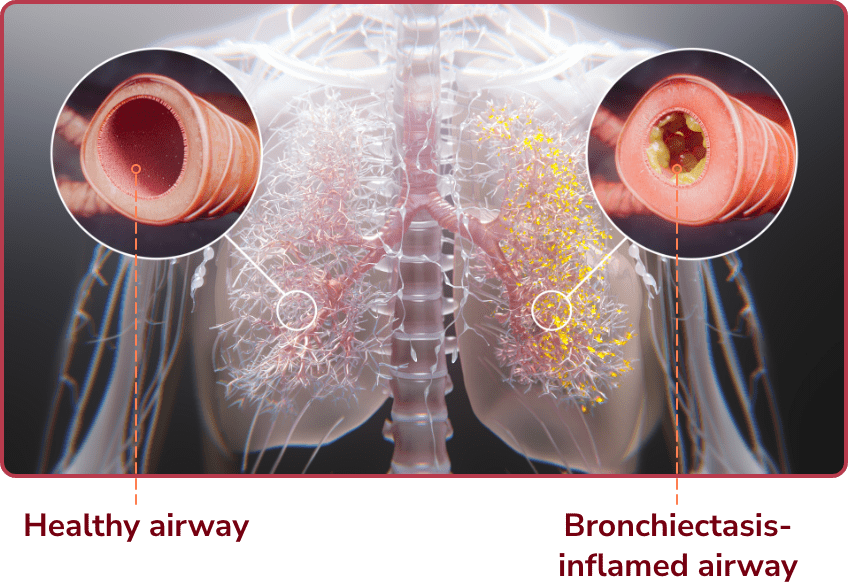
Bronchiectasis is a chronic and progressive lung disease usually marked by permanent, abnormal dilation and persistent inflammation of the airways. 1,2
Bronchiectasis affects approximately 500,000 people in the United States and more globally. 1,3 Although increasing in prevalence, there have long been unmet needs in bronchiectasis. 1,4
The presentation of bronchiectasis often overlaps with other respiratory conditions 5,6
Bronchiectasis initially presents with chronic cough and sputum production in addition to recurrent exacerbations. These nonspecific symptoms mimic more common conditions such as COPD or asthma, which experts believe often delays diagnosis or leads to misdiagnoses. 6-8
Common symptoms associated with bronchiectasis 1,9,10:
- Chronic cough
- Dyspnea
- Daily sputum production
- Fatigue
- Recurrent infections
- Hemoptysis
A definitive diagnosis of bronchiectasis requires both clinical criteria and radiological evidence. 1,7,10
- Clinical suspicion includes presence of symptoms and history of exacerbations
- Findings on imaging include dilated airways, lack of airway tapering, and airway visibility in the periphery
Bronchiectasis has several known etiologies and associated conditions, but up to 40% of patients with bronchiectasis have no specific identifiable cause. 8,11
Exacerbations play a critical role in bronchiectasis disease progression, with serious consequences for patients 12
Patients with bronchiectasis often suffer from periods of worsening symptoms, or exacerbations, which contribute to the burden of disease and can affect patients’ quality of life. 12
Although exacerbations are considered separate from daily symptom burdens, many patients view them as a continuum of the disease and a part of daily life. 13 It’s important that patients are educated about the consequences of exacerbations and the appropriate actions to take, including when to seek medical help.
Identifying an exacerbation
There are no US guidelines that define a bronchiectasis exacerbation. However, a consensus definition from an expert committee defines an exacerbation as a patient experiencing the worsening of 3 or more of these symptoms over 48 hours, requiring a change in treatment 14:
- Cough
- Fatigue and/or malaise
- Breathlessness and/or exercise intolerance
- Hemoptysis
- Sputum volume and/or consistency
- Sputum purulence
Expert commentary: The impact of exacerbations on patients with bronchiectasis
Exacerbations are important for a lot of reasons. One is because patients feel poorly when they have them, and we would therefore like to try and prevent them, or treat them rapidly when they occur. So, we believe that exacerbations are part of what drives the ongoing inflammation and progression of bronchiectasis.
And a lot of that is why we’re trying to prevent these events, to try and prevent that progression of disease. But something we learned is, we tend to focus on the acute things, like the cough and the sputum production, and we measure things like missed days of work or school; and those are all important. But the other thing is these are systemic events. And even though their symptoms of cough or chest complaints may improve rapidly, we actually now have data that show that their physical functioning takes weeks before they recover. And that’s not unlike any other kind of lung infection. And that’s a factor I think we have to pay attention to.
You know, one of the reasons we want to prevent exacerbations is we know they’re associated with some bad outcomes, worsening quality of life, and, very importantly, disease progression, and even mortality. So we really need to focus on preventing these exacerbations for our patients.
When patients have bronchiectasis exacerbations, it may lead to, you know, frequent outpatient visits, frequent hospitalizations, if not treated appropriately, you know, worsening symptoms, worsening quality of life. Oftentimes, they’re trying to help themselves, right? So it leads to more time consumed at home with medical, you know, using certain medications or certain devices. It’s just very cumbersome for the patient when they’re faced with exacerbations. You want to, you know, try to optimize quality of life as best possible for these patients. You know, you want to prevent any sort of worsening lung function from exacerbations or any sort of, you know, worsening inflammation and worsening bronchiectasis, right? So I think it’s very important to identify these exacerbations and treat it appropriately early.
Exacerbations contribute to an increased physical and mental burden for patients with bronchiectasis 1,12
Exacerbations can negatively affect patients and their families, and are associated with 1,12,13:
- Significant anxiety
- Lack of control
- Decreased quality of life
- Embarrassment
- Work and social interruptions
 It’s like waiting for a hurricane—there’s a constant level of fear and anxiety of the unknown. When will an exacerbation hit? How will my life be affected or change with this disease?—Michelle, patient with bronchiectasis
It’s like waiting for a hurricane—there’s a constant level of fear and anxiety of the unknown. When will an exacerbation hit? How will my life be affected or change with this disease?—Michelle, patient with bronchiectasis2x
In a multicenter observational study (N=2,572), patients who had an exacerbation had nearly 2x the risk for another, compared to those who had none. 12
Most patients with bronchiectasis experience 1 or more exacerbations, resulting in greater disease burden over time 15
A retrospective study of US commercial claims and Medicare supplemental core databases included data from 14,798 bronchiectasis patients aged ≥18 years and found that a majority of bronchiectasis patients experienced 15:
- 1 or more exacerbations at Years 1 and 2 of follow-up
- Increased hospitalizations from Year 1 to Year 2
Pulmonary exacerbation* occurrences over time periods in patients with non‑cystic fibrosis bronchiectasis (N=14,798) 15
% of patients
Number of exacerbations:
Pulmonary exacerbation defined here as an inpatient claim with a non-cystic fibrosis bronchiectasis diagnosis or a healthcare interaction, followed by an antibiotic prescription within 7 days. 15
Source: adapted from Flume PA, et al. ERJ Open Res. 2023;9(4):00021-2023.
Copyright ©Flume PA, et al 2023 - This version is distributed under the terms of the Creative Commons Attribution License 4.0.
 I’m always wondering what my tomorrows are going to be like, if they are going to be good or if they are going to be bad. I worry a lot and stress a lot. I have anxiety a lot because I never know.—Erica, patient with bronchiectasis
I’m always wondering what my tomorrows are going to be like, if they are going to be good or if they are going to be bad. I worry a lot and stress a lot. I have anxiety a lot because I never know.—Erica, patient with bronchiectasis